Diagnosis and Analysis
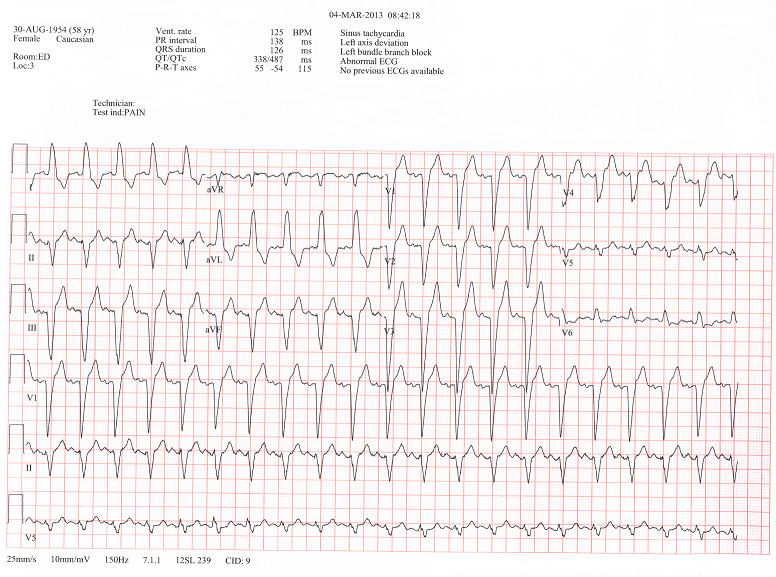
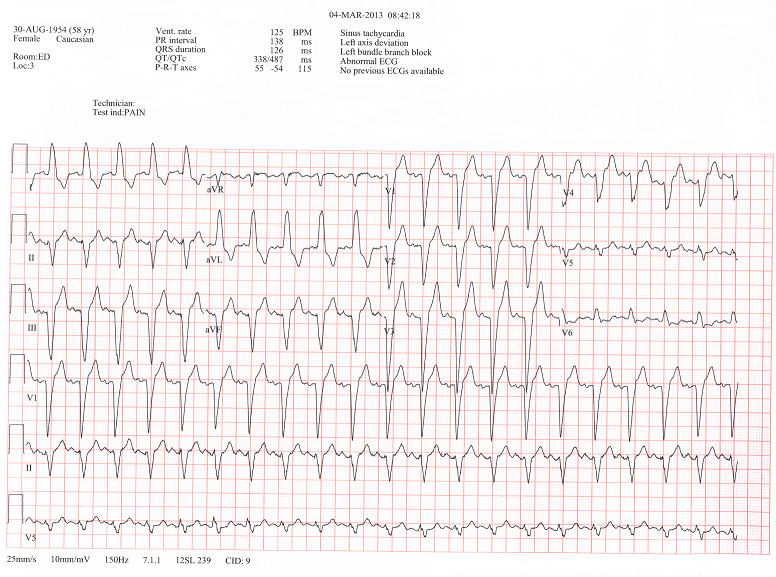
In evaluating her 12 lead we note that she has a left bundle branch block (LBBB). We note this from looking at the V1 lead, if it is .12sec or greater in duration and a negative complex, then using the turn signal indicator method: if the complex is negative (pointing downwards) we push our turn signal indicator in the same direction as the complex. So if our turn signal indicator is pointing downwards, we are turning LEFT, therefore a LBBB. Secondly, we note that the patient has a Left Axis Deviation : a positive complex in Lead I and a negative complex in Leads II and III. It is a good rule of thumb whenever you have a patient with a left axis deviation, to assume that they have an associated left anterior hemiblock, until proven otherwise. We fortunately had the patient's cardiologist in the ED when the patient arrived and was able to let us know that she had a pre-existing LBBB from March of 2013, with a normal heart cath. Here is a copy of her EKG from March.
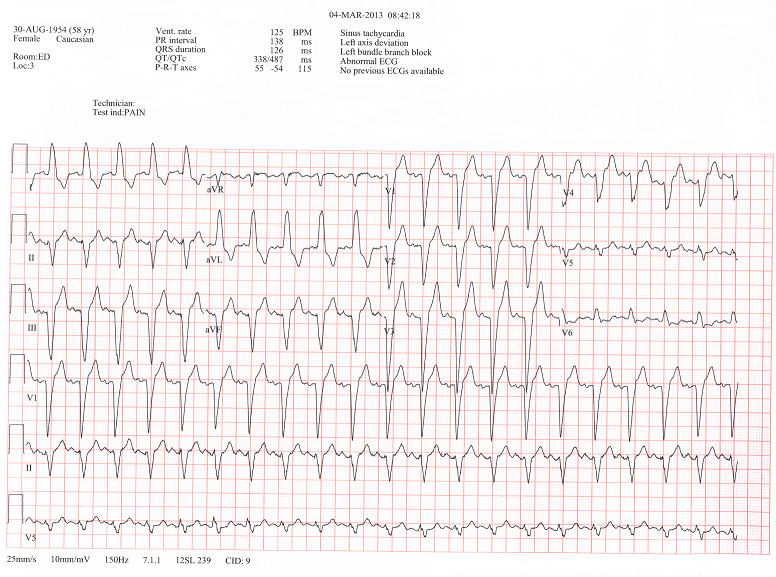
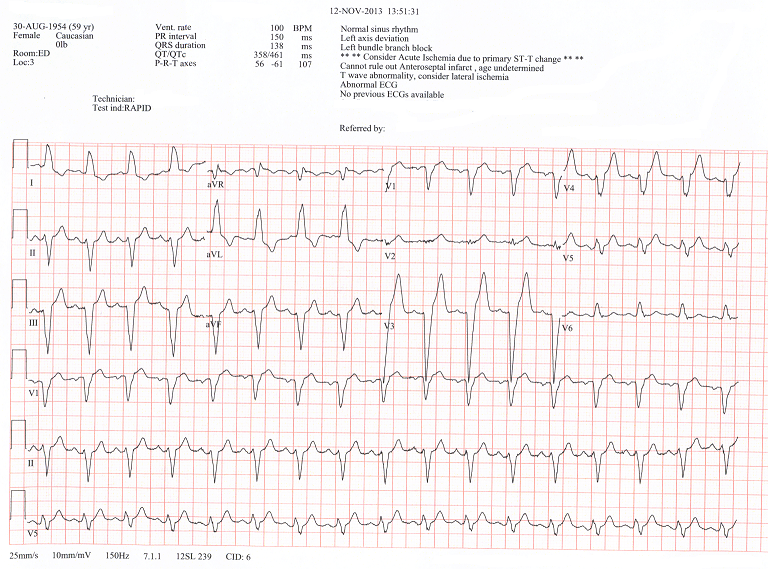
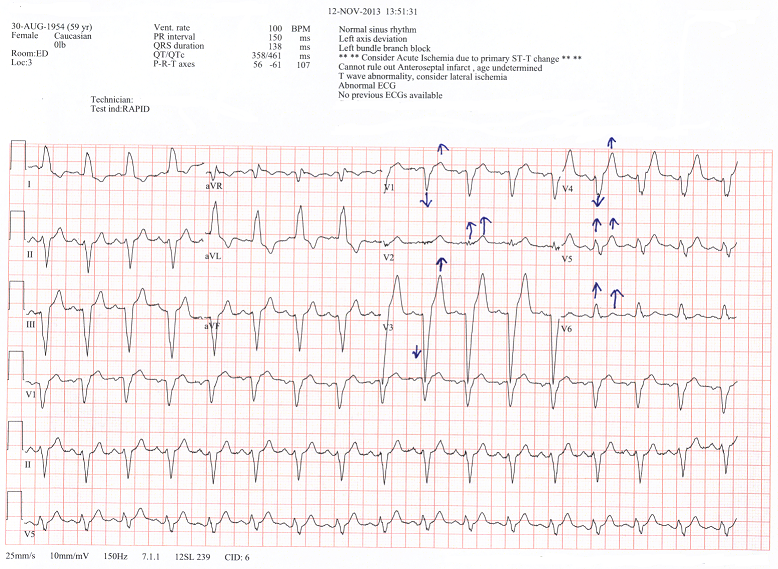
Okay so now go back and evaluate the initial 12 lead EKG on presentation and look at the "old EKG", for comparison.
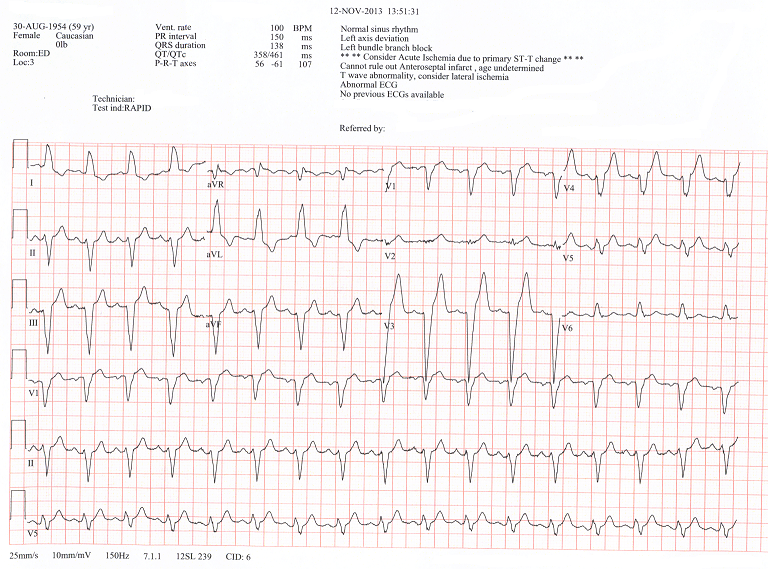
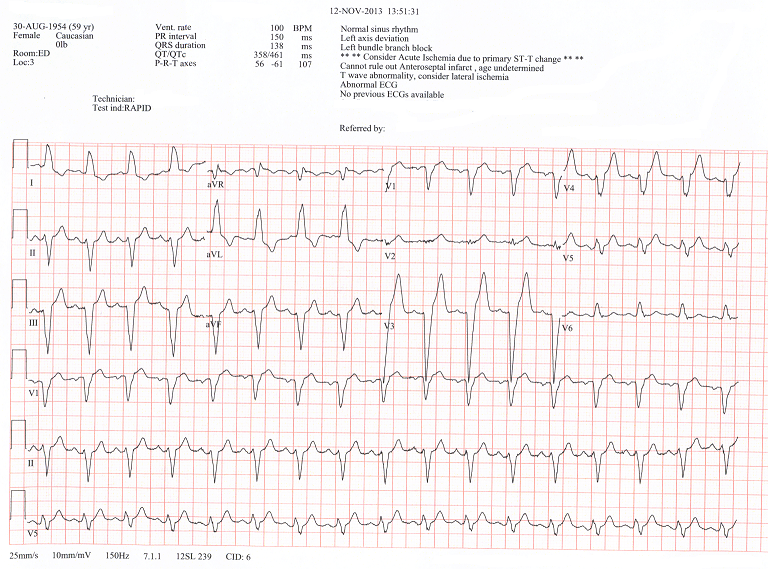
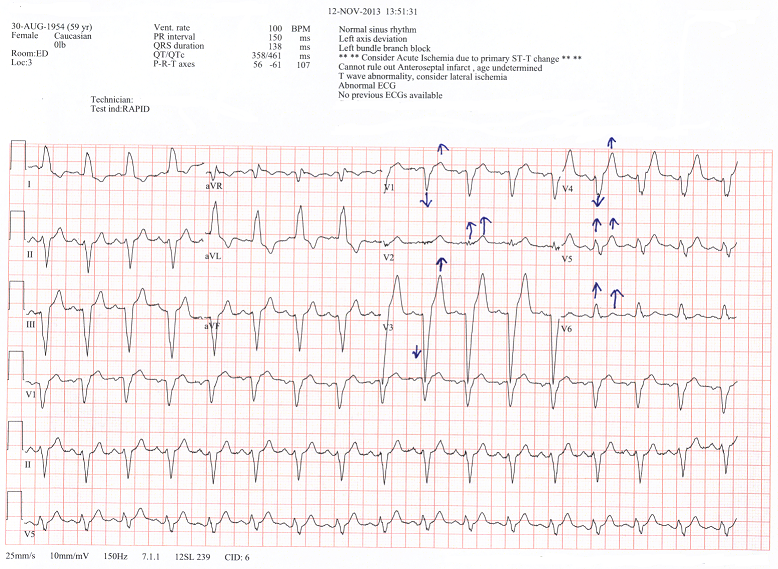
If you look very closely at the first initial EKG you will see some abnormalities in the LBBB pattern. A typical LBBB pattern has a discordant pattern in your chest leads V1-V6. This is to say that if there is a positive QRS, then there will be a negative T wave and if there is a negative QRS, then there will be a positive T wave. Now lets take another look at her initial EKG.
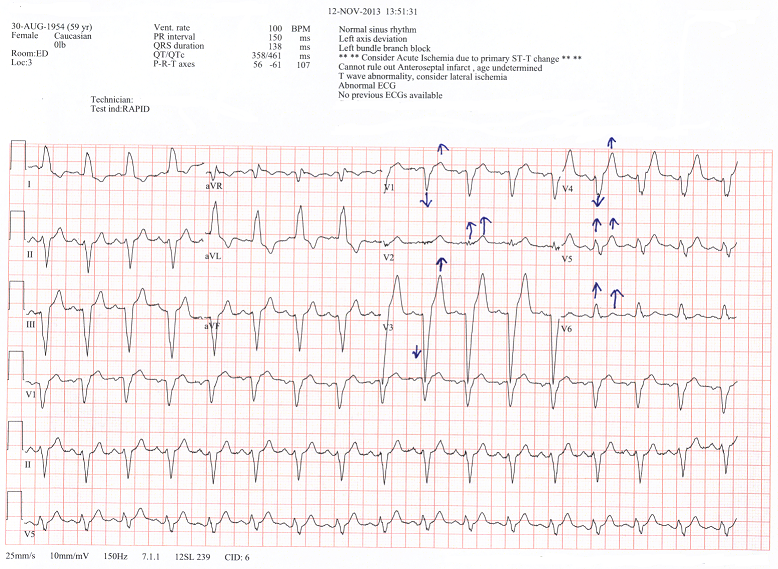
The cardiologist decided to do a 2-D ECHO, because of this abnormal presentation of her LBBB. If you look at leads V2, V4, and V5 it shows a concordant pattern of her QRS to her T waves (note the blue arrows). It showed a new mitral regurgitation that she did not have in March, with some abnormal heart wall motion. She was taken to the cath lab and was found to have a 90% blockage of her Left Anterior Descending (LAD) coronary artery. She received an angioplasty and a stent, opening the blocked vessel.
ANGIOGRAM
CASE FOUR
CASE TWO
CASE ONE